Relieve IBS Symptoms with the Low-FODMAP Diet: A Comprehensive Guide by Dr. Sumaiya
Are you struggling with persistent digestive discomfort, such as bloating, gas, or abdominal pain? If you have Irritable Bowel Syndrome (IBS) or similar digestive issues, the low-FODMAP diet might be the solution you’ve been searching for. This comprehensive guide, developed by Dr. Sumaiya of NutriCare Clinic, provides a clear, evidence-based, and actionable roadmap to understanding and implementing the low-FODMAP diet successfully. This guide is backed by years of experience and scientific research, ensuring a smooth and effective path to better digestive health.
Table of Contents
- What is FODMAP?
- Why Choose a Low-FODMAP Diet?
- The Three Phases of the Low-FODMAP Diet
- Sample Low-FODMAP Foods
- Sample High-FODMAP Foods
- Frequently Asked Questions (FAQs)
- Get Started on Your Journey
- References

What is FODMAP?
FODMAP stands for Fermentable Oligosaccharides, Disaccharides, Monosaccharides, and Polyols. These are short-chain carbohydrates that are poorly absorbed in the small intestine. For individuals with IBS or other digestive disorders, these carbohydrates can ferment in the gut, leading to symptoms like bloating, gas, abdominal pain, and altered bowel habits. According to the Monash University, a leading research institution in this field, approximately 1 in 7 people experience IBS symptoms, and a low-FODMAP diet can significantly improve these symptoms in up to 75% of sufferers.
Why Choose a Low-FODMAP Diet?
The low-FODMAP diet is a scientifically-backed, three-phase approach designed to identify and manage food triggers that contribute to digestive discomfort. It’s not a long-term elimination diet but rather a tool to help you understand your body’s specific sensitivities. Without proper guidance, however, implementing the low-FODMAP diet can be challenging and may lead to nutritional deficiencies. This is why professional supervision by a registered dietitian, like Dr. Sumaiya, is highly recommended.
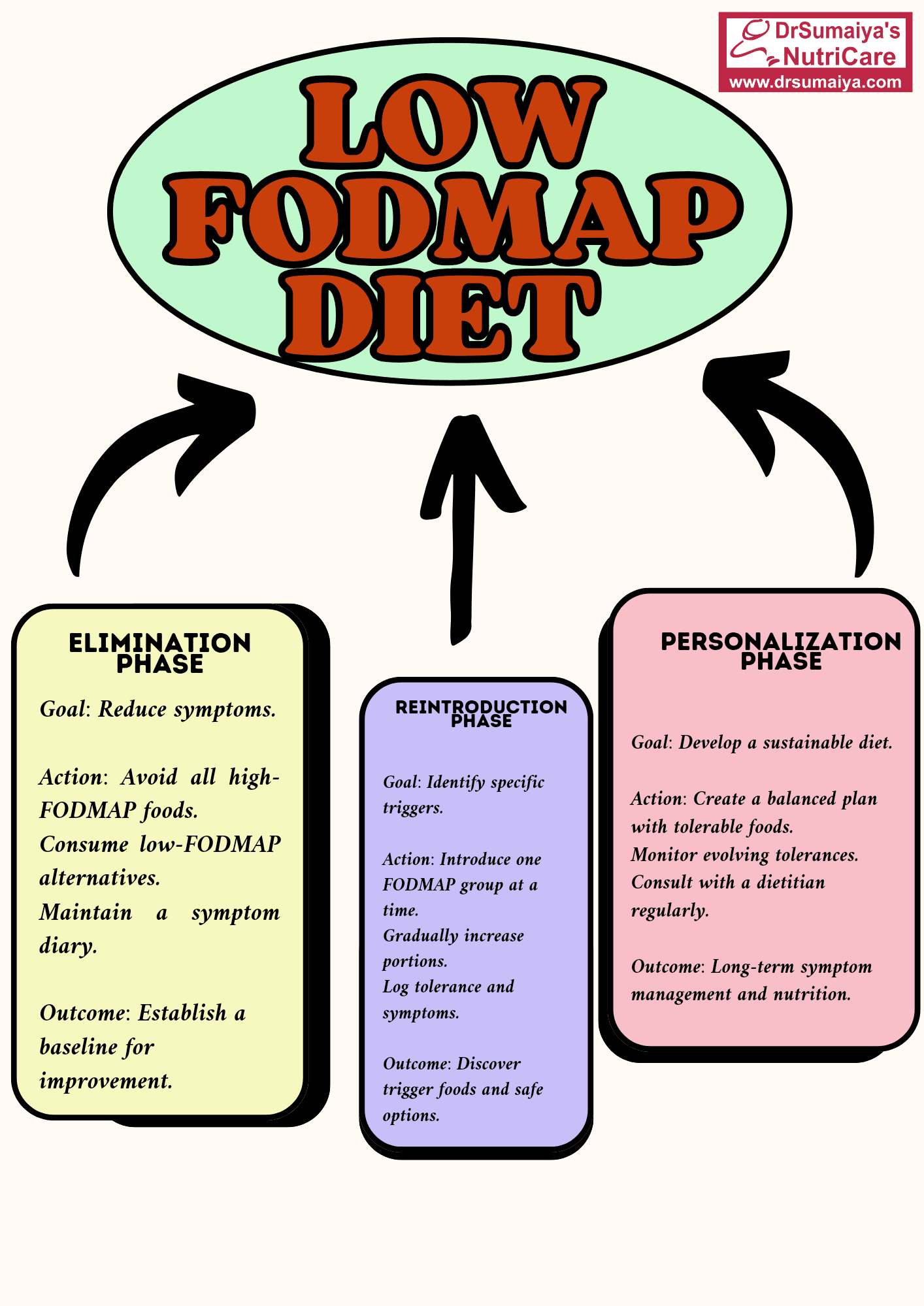
The Three Phases of the Low-FODMAP Diet
1. Elimination Phase (4-6 Weeks)
Goal: To significantly reduce or eliminate high-FODMAP foods from your diet to alleviate symptoms and establish a baseline.
- Action: Strictly avoid all high-FODMAP foods. This includes certain fruits (e.g., apples, pears, mangoes), vegetables (e.g., garlic, onions, asparagus), dairy products (e.g., milk, yogurt), grains (e.g., wheat, rye), and sweeteners (e.g., honey, high-fructose corn syrup).
- Focus on: Consuming only low-FODMAP foods, such as bananas, blueberries, carrots, spinach, lactose-free dairy, and gluten-free grains like rice and quinoa.
- Monitoring: Keep a detailed food and symptom diary to track your progress. Note the foods you eat, portion sizes, and any symptoms you experience (type, severity, and timing).
- Outcome: This phase helps determine if a low-FODMAP diet is effective in reducing your digestive discomfort. Most individuals experience significant symptom improvement within 2-6 weeks.
2. Reintroduction Phase (6-8 Weeks)
Goal: To systematically reintroduce individual FODMAP groups to identify specific triggers and tolerance levels.
- Action: Gradually reintroduce one FODMAP group at a time (e.g., fructose, lactose, fructans, galactans, polyols). Choose one food from each group and consume it in increasing portions over a few days.
- Example: If testing fructose, you might start with a small amount of honey (1/2 teaspoon) on day one, increase to 1 teaspoon on day two, and 2 teaspoons on day three, monitoring for symptoms after each portion.
- Monitoring: Continue to meticulously track your food intake and symptoms in your diary. Note the specific FODMAP group, the food tested, the portion size, and any reactions.
- Outcome: This phase identifies which FODMAPs you can tolerate and in what quantities. It helps pinpoint your individual trigger foods.
3. Personalization Phase (Ongoing)
Goal: To create a long-term, sustainable, and nutritionally balanced diet based on your individual tolerance levels.
- Action: Using the information gathered during the reintroduction phase, design a personalized diet that includes tolerated FODMAPs and avoids or limits trigger foods.
- Flexibility: Your tolerance to FODMAPs may change over time, so continue to monitor your symptoms and adjust your diet as needed.
- Ongoing Support: Regular check-ins with a registered dietitian are recommended to ensure your diet remains balanced and to address any concerns or changes in your symptoms.
- Outcome: A long-term, personalized diet plan that minimizes digestive symptoms while ensuring you receive adequate nutrition and enjoy a variety of foods.
Sample Low-FODMAP Foods
| Food Group | Examples |
|---|---|
| Fruits | Bananas, blueberries, strawberries, grapes, oranges |
| Vegetables | Carrots, spinach, zucchini, bell peppers, eggplant |
| Grains | Rice, quinoa, oats (check for gluten-free certification if needed) |
| Protein | Chicken, fish, tofu, eggs |
| Dairy/Alternatives | Lactose-free milk, hard cheeses, almond milk |
Sample High-FODMAP Foods
| Food Group | Examples |
|---|---|
| Fruits | Apples, pears, mangoes, watermelon, dried fruits |
| Vegetables | Garlic, onions, asparagus, cauliflower, mushrooms |
| Grains | Wheat, rye, barley |
| Legumes | Beans, lentils, chickpeas |
| Dairy | Milk, yogurt, ice cream |
| Sweeteners | Honey, high-fructose corn syrup, agave |
Frequently Asked Questions (FAQs)
- 1. What is the low-FODMAP diet, and who should try it?
The low-FODMAP diet is a structured approach to reducing digestive symptoms caused by poorly absorbed carbohydrates. It’s primarily recommended for individuals diagnosed with IBS or similar functional gastrointestinal disorders. A proper diagnosis is crucial before starting the diet.
- 2. Can I follow a low-FODMAP diet without a dietitian?
While it’s possible to find information online, it’s strongly *not recommended* to undertake the low-FODMAP diet without professional guidance. A registered dietitian ensures nutritional adequacy, helps you navigate the complex three-phase process, and provides personalized support to minimize the risk of nutrient deficiencies and unnecessary restrictions.
- 3. How long does it take to see results?
Many individuals experience a noticeable improvement in their digestive symptoms within the first 2-6 weeks of the elimination phase. However, the full process, including reintroduction and personalization, takes several months.
- 4. Are there risks associated with the low-FODMAP diet?
Yes, if not implemented correctly. Potential risks include nutrient deficiencies (especially fiber), increased anxiety around food, disordered eating patterns, and unintended weight loss. Working with a registered dietitian minimizes these risks.
- 5. Can I ever eat high-FODMAP foods again?
Yes! The reintroduction phase is specifically designed to help you identify which FODMAPs you can tolerate and in what quantities. The goal is not to permanently eliminate all high-FODMAP foods but to find a balance that minimizes symptoms while allowing for dietary flexibility.
- 6. What are some examples of low-FODMAP foods?
See the table above for examples. Common low-FODMAP options include bananas, blueberries, carrots, spinach, zucchini, lactose-free dairy, gluten-free grains (rice, quinoa), and lean proteins.
- 7. How do I track symptoms effectively?
Use a detailed food and symptom diary. Record everything you eat and drink, including portion sizes and ingredients. Note the time of meals and any symptoms you experience (type, severity on a scale of 1-10, and timing). This information is invaluable for identifying trigger foods.
Get Started on Your Journey to Better Digestive Health
Starting a low-FODMAP diet can be a significant step towards improving your digestive health and overall well-being. However, it’s crucial to remember that this journey is best undertaken with the support of a qualified healthcare professional. Dr. Sumaiya, a Registered Dietitian at NutriCare Clinic, has extensive experience guiding patients through the low-FODMAP diet.
Take control of your digestive health today! Fill out our patient history form to schedule a consultation with Dr. Sumaiya and receive personalized guidance on implementing the low-FODMAP diet.
References
- Monash University FODMAP Diet. https://www.monashfodmap.com/
- Barrett, J. S. (2017). How to institute the low-FODMAP diet. *Journal of Gastroenterology and Hepatology*, *32*(Suppl 1), 8–10. https://doi.org/10.1111/jgh.13686
- Tuck, C. J., Muir, J. G., Barrett, J. S., & Gibson, P. R. (2014). Fermentable oligosaccharides, disaccharides, monosaccharides and polyols: role in irritable bowel syndrome. *Expert Review of Gastroenterology & Hepatology*, *8*(7), 819–834. https://doi.org/10.1586/17474124.2014.917956